In oncology discovery, AI is changing our understanding of cancer. What had previously taken long years of lab work can now be discovered within a few days and researchers can uncover the previously unseen genetic patterns and the drug targets we had never looked at before. That would be expediting science and setting the new bar for medicine.
The genetic chaos of tumors has puzzled many scientists for generations. But finding these specific molecular targets, which truly cause the disease – it has been a slow and sometimes uncertain process to do so. Now, AI can uncover hidden patterns in biology hidden away from sight, drawing together hints from thousands of works and revealing insights that humans cannot. This process seems particularly difficult for genetic researchers, such as those working with tumors.
As the next generation of AI-powered physicians, cancer researchers have transitioned from trial-and-error drug discovery to smarter, accuracy-driven methods of discovering things in order to prevent the problem. As a partner with AI in our team, our progress in cancer therapy transitions from trial-and-error drug discovery to better-informed, precision-driven research in which every piece of discovery is one more piece closer and closer towards the kind of personalized treatment you never knew would be possible.
Building “Single Target for Cancer”
To address this challenge of finding cancer-specific therapeutic targets, we created the “Single Target for Cancer” workflow — an AI-driven framework to discern genuine biological signal from noise.
Contrast with past bioinformatics tools, which trained on static rule sets, this one can employ contextual learning-based techniques to detect the patterns in gene behavior for the cancerous and healthy tissues. The goal is to isolate molecular targets, which are active in tumors but silent in normal cells.
Instead of searching for statistical anomalies, the system learns from the biological context — how a gene works, interrelates, and contributes to the creation of disease. That allows scientists to make progress from correlational to causal and to track down targets that are clinically relevant and therapeutically helpful.
Key Steps: From Data to Discovery
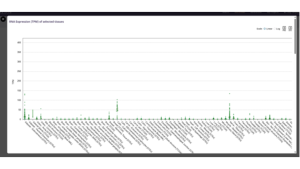
1. Cancer vs Healthy Tissue Expression Comparison. Using large-scale datasets (TCGA, GTEx, and Beat AML), the algorithm analyzes gene expression across tumor and normal samples to determine where a gene “switches on” or “off.”
2. Measuring relevance, not just difference. Each gene gets a differential expression score, which quantifies both the strength and direction of its activity.
- Positive scores → overexpressed in tumors (potential cancer drivers).
- Negative scores → mean the gene is more active in healthy tissue.
The algorithm doesn’t just detect change, it assesses biological relevance, calling attention to genes most likely associated with disease mechanisms.
3. Filtering for Specificity. User-defined thresholds ensure to only retain genes that are very active in cancer but present at a slim scale in healthy tissue. This reduces false positives and guides us towards genuinely selective therapeutic targets.
It is just part of the set of tools that together create a focused map of candidate drug targets and biomarkers — the basis of less toxic, selective cancer therapies.
In oncology research, the most effective and safest therapies are those that differentiate malignant cells from healthy ones — attacking the disease selectively and sparing normal tissue. That’s exactly what this workflow was designed for.
Such precision-based methodology is not only considered good practice, but also enables scientists and pharmaceutical developers to optimize time- and resource-saving efforts by honing in on targets that, while powerfully consequential in cancer, are also essential to everyday life, a common driver of side effects and trial failures.
From Data Chaos to Clarity
The workflow is already delivering actual results. In a pilot study with almost 30,000 tumor and healthy tissue samples from multiple types of cancers, it identified the most probable candidate genes with unique cancer-specific expression signatures, several of which are currently being tested for the development of drugs. The AI feature greatly increased efficiency:
- Data disambiguation accuracy reaches 67%. So that it can correctly read both biomedical and overly technical terminology in the majority of scenarios.
- 27% reduction in useless or confusing findings, giving researchers the opportunity to focus on interesting leads faster.
- Recorded 93–96% knowledge precision, a level of precision achieved by AI in contextualizing gene-disease relationships arising from the merging of structured and unstructured data.
By combining language models (e.g., BERT) with big biomedical databases, the system can understand not only which concepts are actually related, but also understand how the concepts are connected in context, linking up the raw data with the scientific meaning.
Models can be trained to identify and combine information into a cohesive schema that allows researchers to merge newer sources of genomic, proteomic and bibliographic data into a unified database. This development has massively sped up the process on-boarding new datasets and improved general scale for discovery workflows.
AI works, then, as an invisible infrastructure — not just analyzing but also selecting and aligning the scientific universe to drive higher-order discovery.
Ethical and Practical Considerations
Transparency and fairness are important in healthcare, as they are in any kind of AI. Data bias issue is still a major issue—Genomic datasets will not cover every population evenly, and thus predictions could be distorted. Further, even though AI can speed new discoveries, it needs to be interpretable – scientists need to understand why a model suggests a target or therapy.
AI in precision medicine enhances human insight while relieving scientists of the need to repeat analytical processes, allowing them to focus on reasoning, creativity and validation.
The Road Toward AI-Driven Precision Medicine
The future of precision medicine, as it appears, is to combine human insight and machine insights. As AI continues to learn from genomic, clinical, and molecular data, it will no longer only predict disease, it will help prevent it.
Doctors will stop responding to illness. They will start to anticipate it, empowered by AI tools that can track small biological changes well before they begin to emerge. This vision extends far beyond cancer. The principle that we learned from discovering oncogenic drivers can have the same potency for tackling autoimmune, metabolic and neurological diseases by opening up access to medicines made by patients depending on their own unique molecular signature.
But progress has to be accompanied by ethics. Evidence for trust in AI in healthcare will rely heavily on a range of data, interpretability, and transparency. Precision medicine must be more than mere technological sophistication. It must be equitable, inclusive, and humane.
AI will not replace the scientists or the clinicians, it will enable them. The greatest breakthroughs will be among people, not algorithms, but the interplay of human intuitive skills and advanced artificial intelligence to make medicine truly personal.
Closing Note
Precision medicine does not aim for a universal cure that fits all people. Its ultimate goal is to find something that hits the right target for the right patient. AI has allowed scientists to accomplish this more quickly, more precisely and more safely than ever before.
But like any scientific revolution, it’s at its best when it’s collaborative; across data scientists and clinicians, between open data sets and proprietary algorithms, and, most importantly, between human insight and machine intelligence. AI helps us think more effectively, and in drug discovery this distinction could set the difference between a failed trial and the next life-saving therapy.