
AI technology that monitors patients for early signs of deterioration could free up much needed critical care beds and increase overall surgical capacity
The impact of COVID-19 on the NHS, and especially on critical care units, has been immense and has resulted in unprecedented pressure on surgery waiting lists. Transitioning patients in and out of critical care units safely and efficiently is going to be key to clearing this backlog and getting patients the treatment they need. Patient monitoring systems that use Artificial Intelligence (AI) to flag early warning signs for patient deterioration in critical care settings could be a key tool to help clinicians to improve outcomes and reduce critical care length of stay for patients.
Patient monitoring in critical care
Effective early warning systems for patients in critical care are not routinely used but could guide prompt interventions to improve patient outcomes and safety. There are also huge potential cost savings, not only because reducing complications leads to shorter hospital stays and less resource consumption, but also because low-risk patients can be identified early and transitioned out of critical care.
Unfortunately, available early warning score models currently used in most critical care settings are severely limited by their static nature and generic thresholds. These limitations mean that they can fail to identify subtle signs of patient deterioration until it is too late. In contrast, AI-driven technology has the potential to transform early warning systems, as it can anticipate patient deterioration in real-time and allow clinicians to take proactive preventive action.

Although cardiac surgery outcomes have improved significantly over recent years there remains a significant risk of complications. Approximately 3 percent of patients will not survive the surgery. Complications after cardiac surgery rapidly evolve and therefore any tool which can alert the clinical team to a developing complication before it occurs has the potential to positively impact patient outcomes. Artificial Intelligence and machine learning are capable of analysing the vast amounts of patient data collected in intensive care to make these tools a reality.
So, what is holding critical care teams back from embracing AI-driven patient monitoring solutions?
Challenges of deploying AI in critical care
Despite the broad acceptance that AI technology will have a strong role to play in critical care settings, there are still a number of challenges that are delaying deployment.
Firstly, the lack of AI-driven technology platforms that are proven in real-life clinical settings means that there is healthy skepticism around new platforms promising extraordinary results. It is right that any new technology needs to be rigorously investigated and tested, but we shouldn’t let our desire for certainty get in the way of innovation. There are low-risk ways to test new technology platforms with real patients without compromising safety, and we should be open to these opportunities.

This skepticism also plays into the reluctance some healthcare teams have of being the first to deploy new technology. Additional care and heightened security are always necessary when analysing patient data. Clinicians can be wary of new platform technologies and often perceive them as too high-risk. However, many AI-driven technology platforms can now operate securely and locally, without needing to access any identifiable patient data.
Finally, there are always implementation concerns when it comes to new technology platforms within hospitals and critical care. To achieve wide adoption, new technologies need to blend seamlessly with existing clinical pathways, fully integrate with existing IT infrastructure and interface with relevant data streams.
Systems that add to the workload of already overstretched healthcare teams are not fit for purpose, and nursing teams absolutely have to find the technology both easy-to-use and beneficial to themselves and their patients. Happily, these concerns are widely acknowledged, and much of the new technology is being developed with this in mind.
How does AI-driven patient monitoring work?
One AI-driven patient monitoring system which has been successfully deployed in a critical care setting is the STABILITY platform, developed by UK start-up Rinicare. A product evaluation at Wythenshawe Hospital, part of Manchester University NHS Foundation Trust, is currently underway to assess the platform amongst cardiac surgery patients in its Cardiothoracic Critical Care Unit.
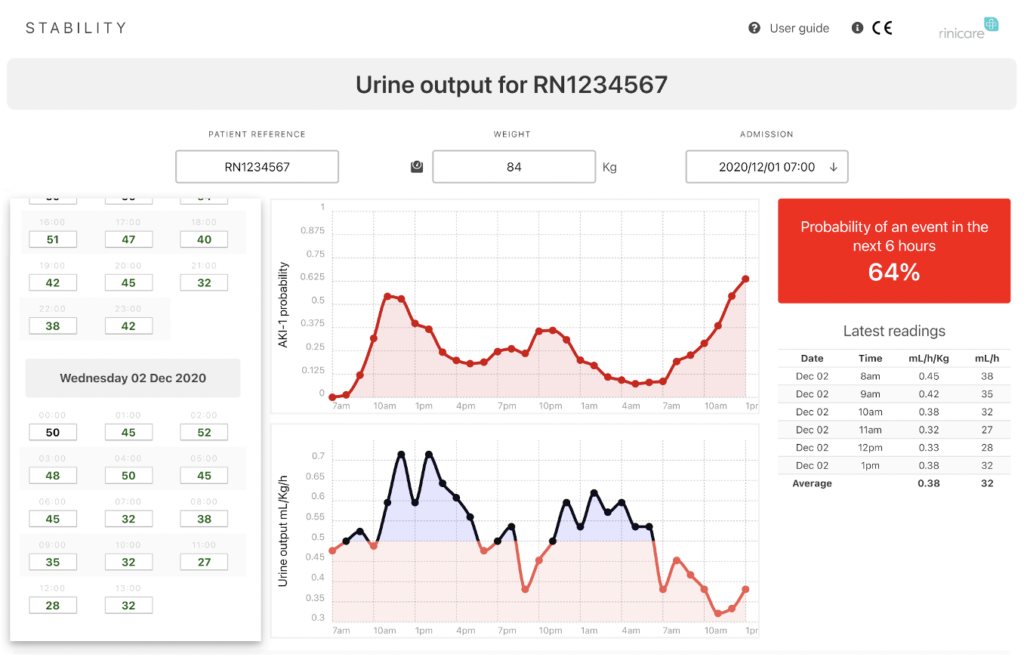
The first offering available on the STABILITY platform is STABILITY UO (urine output), a CE-marked software solution developed to predict the risk of developing renal complications or acute kidney injury (AKI) after cardiac surgery. Powered by a clinically validated algorithm, STABILITY UO’s predictive power has been shown to accurately predict dangerous episodes of low urine output that, without intervention, correlate strongly with increased morbidity and mortality.
Acute Kidney Injury (AKI) is a major healthcare burden, estimated to cost the NHS alone £1.02 billion per year, and is a particular concern for clinicians managing cardiac patients following surgery. AKI occurs in up to 12 per cent of patients in general undergoing surgical procedures and about a third of patients following cardiac surgery.
Using routinely taken physiological measurements routinely, STABILITY UO can predict the future probability of low urine output in time for clinicians to take preventive action to reduce the risk of developing AKI. This risk prediction is personalised for each patient, is available after only six hours of post-operative monitoring and is updated hourly.
A vital aspect of the STABILITY UO platform for clinical teams is that it can be integrated into the hospital’s local IT network, and then accessed seamlessly through bedside monitors, nursing PCs or tablets. This allows nurses to input the regular urine output readings without major disruption to their routine.
Data from the Wythenshawe Hospital product evaluation should be available later in 2021, demonstrating the impact that AI-driven patient monitoring can have on high-risk critical care patients. The Rinicare team is also developing new applications for the STABILITY platform. The next offering focuses on postoperative atrial fibrillation (AF) which affects up to one third of patients after cardiac surgery. Rates of postoperative AF have remained stubbornly high for decades, so this is another really exciting area for the application of AI-driven technology.
Putting the clinician at the heart of AI
There are many understandable and valid concerns about ceding clinical control to AI-driven technology in healthcare, which is why clinicians need to be kept at the heart of any new technologies. With AI-driven early warning systems, this means using AI to detect small but meaningful changes in a patient’s physiological data that then allow clinicians to act quickly and effectively. In this way, AI is used to enhance a clinician’s decision-making but leaves the clinician firmly in control of decisions about patient care.
The potential benefits of clinical risk prediction technology for the NHS during this crucial recovery phase from the pandemic are far-reaching, and could have an almost immediate effect on the number of surgeries a critical care unit has the capacity for. The ongoing evaluations of solutions like STABILITY show that we are fast approaching the point where patients and clinicians can both start to truly appreciate the benefits of AI technology in the healthcare setting.



