With hundreds of rural hospitals at risk amid tightening policy and payer pressure, administrative work that generates no revenue is rapidly becoming a survival issue—not just an inconvenience. MedEvolve’s new revenue cycle benchmarks measure and eliminate wasted work touches so rural facilities can regain capacity, stabilize cash flow, and protect the patient’s access to care.
SAN FRANCISCO, Feb. 2, 2026 /PRNewswire/ — Rural hospitals are being pushed to the brink by forces largely outside their control—shifting federal policy, payer pressure, and weak negotiating power. But another big threat is hiding in plain sight, quietly consuming the resources rural facilities can least afford to lose: administrative work that generates no revenue.
The American Hospital Association is raising the alarm that hundreds of rural hospitals are at risk of extinction under shifting federal policy and mounting financial pressure. A recent Business Insider report tracked 100+ rural hospitals that have already closed since 2005, meanwhile recent federal regulation, namely OBBBA, is putting ERs, maternity wards, and inpatient services at high risk of being shut down. The ensuing cuts to Medicaid will only lead to more closures and uninsured patients.
No Room for Inefficiencies
These disadvantages are exactly why administrative waste is a closure accelerant rural hospitals can’t afford, according to Matt Seefeld, CEO of MedEvolve. “Most administrators on the provider side are touching claims multiple times. We calculate at least 63% of those touches are wasted effort due to inefficiencies and ‘payer games.’ Follow-ups create a snowball effect of red tape and waste,” Seefeld said. “In an environment where rural providers are often disadvantaged in commercial negotiations, there is even less of a cushion when costs rise. Every hour lost to avoidable work becomes a margin event.”
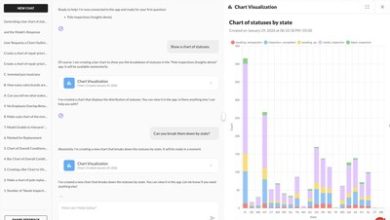
MedEvolve’s Effective Intelligence® (Ei) Technology suite gives healthcare organizations the first actionable visibility into human work effort—pinpointing where administrative waste originates, what it costs, and which “touches” can be eliminated quickly without cutting staff or services.
“When administrative work multiplies, it doesn’t just frustrate teams—it slows cash flow, strains staffing, and threatens access,” Seefeld said.
Rural Hospitals Face Grim Reality
Healthcare policy debates often focus on reimbursement rates, patient out-of-pocket spending and labor shortages, but rural hospitals face a greater threat: The increasing squeeze from an operational reality that traditional systems and metrics fail to capture—compounding costs of manual administrative effort. Recent research published in Health Affairs Scholar shows that administrative cost dynamics differ between urban and rural hospitals, with smaller, rural hospitals devoting as much as 19% more on administrative and general (A&G) salaries.
At the same time, administrative transactions and billing-related work remain a major national cost driver. According to the Council for Affordable Quality Healthcare (CAQH), medical administrative spend reached $82.7 billion in 2023, with providers shouldering 97% of those costs. Denials amplify the workload further. Optum’s 2024 Revenue Cycle Denials Index found an average denial rate of 12% for hospital claims—reflecting the scale of manual follow-ups and rework required to get paid.
Touch-level Benchmarks: Wasted Work Visible and Removable
Traditional industry standards such as days in A/R, net collection rate, and clean claim rate have long been used to signal financial performance and timely payment. But these benchmarks reflect outcomes after the fact. MedEvolve goes further, asking more fundamental questions like: “How much work did the claim require before it left the office?” By shifting benchmarking from lagging indicators to leading measures of labor effectiveness—zero touch rate, avoidable touches, denials-related effort, and first-touch payment—organizations can identify inefficiencies before they impact margin.
MedEvolve’s touch-level benchmarks are a key part of a revenue cycle workflow intelligence that quantifies where administrative burdens originate and what they cost, down to each touch. This functionality gives healthcare organizations a measurable path to eliminate wasted work and stabilize operations.
“Healthcare keeps trying to solve a cost crisis while ignoring the biggest controllable driver: wasted work,” Seefeld said. “If you’re not measuring human work, you can’t manage it. That’s exactly what we’re doing—measuring the work down to the touch—and giving leaders the true data and the tools they need to quickly eliminate administrative waste, restore margins, and relieve burnout.”
Unlike legacy Practice Management and Electronic Health Record reporting tools that measure outcomes after the fact, MedEvolve analyses human effort as a leading indicator—revealing where time is being consumed, where rework is originating, and where touches are avoidable.
Administrative waste isn’t only a finance problem—it’s a capacity problem that seeps in and hits hardest in community and rural hospitals when staff spend their day on repetitive, low-value work.
“Burnout isn’t a mystery, and it isn’t inevitable—it’s what happens when highly trained teams spend their days doing low-value work no one can see or stop,” said Seefeld. “The system can’t fix what it fails to measure; we measure it, and we fix it.”
Key outcomes include:
- Touch Benchmarking: Establishes clear, measurable efficiency standards and shows where manual touches persist by function, department, and site.
- Avoidable Touch Elimination: Identifies non-value work and pinpoints root causes—so teams stop rework instead of managing it.
- Faster Margin Recovery: Removes waste without layoffs or service cuts by freeing capacity and reducing needless labor spending.
- Burnout Reduction: Shifts staff time away from repetitive tasks and toward higher-value work that supports patients and clinicians.
- Better Patient Experience: Reduces billing friction and administrative delays that frustrate patients and slow access.
“Leaders don’t need another report telling them what they already know – that margin erosion is a problem,” said Seefeld. “They need a way to locate wasted work precisely, remove it quickly, and prove the impact. That’s what these benchmarks deliver.”
Cut Costs, Not Services
MedEvolve is positioning itself as healthcare’s truth-teller on administrative waste. By quantifying human effort, their solution enables healthcare organizations to compare performance across departments and locations, prioritize workflows with the fastest operational ROI, and turn waste elimination into a repeatable discipline—not a one-time initiative.
Demonstrations of MedEvolve’s platform and Zero-Touch benchmark approach are available for health leaders, revenue cycle executives, and hospital operations teams. “Healthcare should be focused on patients—not paperwork,” Seefeld said. “We’re exposing the hidden tax of wasted work and helping hospitals eliminate it so teams can get back to care.”
About MedEvolve
MedEvolve is rewriting the rules of the revenue cycle, helping healthcare organizations move beyond labor-intensive, reactive reimbursement work. Its Effective Intelligence® (Ei) platform provides visibility into the operational activity behind reimbursement, enabling leaders to identify avoidable effort, streamline workflows, and support scalable automation. By reducing unnecessary touches and improving process control, MedEvolve helps organizations accelerate resolution, increase predictability, and operate more efficiently in an increasingly complex payer environment. Learn more at https://MedEvolve.com.
References
- Council for Affordable Quality Healthcare. (2024). 2023 CAQH Index report: Measuring the cost of conducting administrative transactions in the healthcare industry.
- Kelly, Allie, Business Insider, (January 19, 2026), Hundreds of America’s rural hospitals have vanished. Maps show closures by state.
- MedEvolve. (n.d.). Effective Intelligence®: Revenue cycle automation with real-time, AI-powered insights to reduce cost to collect, measure employee performance, and increase labor capacity. MedEvolve. medevolve.com/rcm-pm-solutions/effective-intelligence/
- Optum. (2024). The Optum 2024 revenue cycle denials index.
- American Medical Association. (2024). 2024 AMA prior authorization (PA) physician survey.
- American Hospital Association. (2025, June 12). Analysis: Rural hospitals at risk due to cuts in OBBBA. AHA News.
- Handlon, L., Simpson, K., Leaming, L., & Williams, D. (2025, August 8). Trends in hospital administrative costs: Urban–rural disparities, barriers, and reduction strategies. Health Affairs Scholar
- Semuels, A. (2025, July 2). The surprising reason rural hospitals are closing. TIME.
Media Inquiries:
Karla Jo Helms
JOTO PR™
727-777-4629
jotopr.com
View original content to download multimedia:https://www.prnewswire.com/news-releases/the-quiet-rural-hospital-killer-wasted-work-drains-margin-and-depletes-staff-capacity-302676305.html
SOURCE MedEvolve