The healthcare industry is in the midst of an AI arms race to rapidly adopt the latest and most competitive artificial intelligence (AI) technologies aimed at increasing efficiency and reducing costs, while simultaneously improving patient outcomes. While AI-driven solutions are created with the promise of improved workflows and decision-making capabilities for healthcare providers, the pressure to adopt these tools quickly has caused hospitals and health systems to prematurely implement solutions, sometimes without clear expectations. This leads to an increasingly alienated clinical workforce and a lack of clear return on investment (ROI) for the organization.
The rapid adoption of AI tools in healthcare has created challenges in balancing innovation with provider and patient needs while integrating technologies into existing workflows without disrupting care delivery. There are several key factors that healthcare organizations should consider when it comes to keeping up with the race to adopt the most advanced and effective AI technologies.
The Struggle to Achieve ROI in AI Investments
The excitement around AI adoption in healthcare is infectious and often leads organizations to seek out what they believe to be necessary solutions for their staff and patients, but many health systems fail to achieve a meaningful return for several reasons. A common issue is the reliance on seemingly never-ending pilot programs without a clear roadmap for scaling solutions organization-wide. This “pilot-itis” leads to stagnation where AI tools remain in testing phases without ever reaching full-scale deployment.
Excessive pilot programs can stall AI adoption in healthcare because they fail to address unique industry challenges such as regulatory compliance with HIPAA or potential workflow disruptions that could impede patient care when clinicians struggle with already-high administrative burdens. Additionally, hospitals and health systems face data integration concerns due to fragmented and confidential data across electronic health records (EHRs) that make AI implementation complex. Many organizations fail to vet potential tools for their impact on existing processes or their ability to support expanding technology beyond the pilot phase. Failure to complete a thorough evaluation can result in more complexity when the intent is to streamline operations.
Lack of stakeholder engagement further compounds the implementation problem. The success of new AI technologies requires buy-in from senior leadership, operational staff, IT and–most importantly–the clinical workforce. When clinical stakeholders are not actively involved in the decision-making process, it can lead to resistance and skepticism that hinders adoption.
Another critical challenge is the absence of organizational change management (OCM), which can cause AI initiatives to struggle to gain traction due to insufficient training and ongoing support. Without clinical leader buy-in and a clear focus on improving patient outcomes, AI initiatives risk becoming technology-centric rather than patient-centered innovations.
Integrating AI Without Disrupting Workflows
For AI to be successfully integrated into healthcare workflows, clinical leadership must be involved early in the process to document, socialize and obtain agreements on the current state of workflows, including all exceptions and optional scenarios. Early involvement not only ensures that AI tools address real, quantifiable problems, but it also creates a sense of ownership and involvement that ultimately increases staff members’ willingness to participate in and adopt the new technology.
Provider organizations need to define the specific clinical or operational challenge an AI tool is meant to address to ensure it supports, rather than complicates, existing workflows. A key way to do this is through evaluation. Similar to clinical trials that quantify the effectiveness of medical treatments, healthcare providers must measure the performance of AI solutions and meticulously evaluate metrics that demonstrate a digital tool’s impact on efficiency, patient care and cost savings on an ongoing basis.
It is also beneficial to conduct focus groups with patients that go beyond typical experience surveys and evaluations. Patients are one of the most overlooked stakeholders in the AI implementation process, creating an opportunity for hospitals and health systems to ask the right questions to determine which technologies patients find valuable and identify what they liked or disliked during their previous interactions with the healthcare system to better tailor AI solutions.
Prioritizing interoperability is another crucial element in mitigating disruptions. AI tools must integrate seamlessly with existing systems to limit disruptions and reduce administrative burdens on clinical staff. This is achieved through collaboration between IT teams and clinicians to establish proper data management, training and ongoing support.
Scaling solutions is considerably more difficult if the organization has insufficient resources and lacks personnel with the knowledge and skills to support an enterprise-wide implementation or a secure long-term funding plan through a governance structure. By considering each of these elements proactively, provider organizations can integrate AI in a way that enhances rather than hinders patient care.
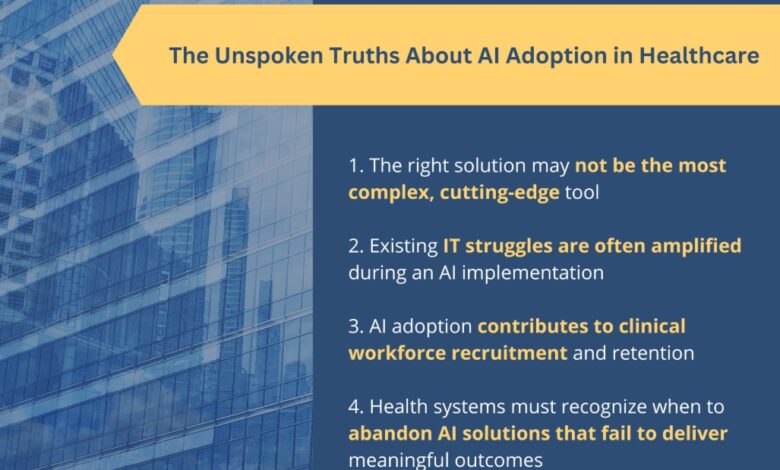
The Unspoken Truths About AI Adoption in Healthcare
While AI is a necessary step toward modernization, the solution may not always be the most complex, cutting-edge tool. It is crucial to determine the appropriate level of complexity and features of new tools in alignment with the skills, capabilities and preferences of the clinicians who will be using them. AI and digital tools must solve a real problem or pain point–or it risks negatively impacting patient care.
Often, existing IT struggles are amplified during an AI implementation. If a health system already faces operational inefficiencies, cybersecurity vulnerabilities or interoperability issues, adding AI into the mix may only worsen these problems. Addressing foundational technology gaps before implementing AI is crucial to preventing additional issues.
AI adoption also contributes to clinical workforce recruitment and retention at a time when healthcare systems are experiencing an unprecedented labor shortage. New healthcare professionals are drawn to organizations that leverage cutting-edge technologies to improve care delivery, while health systems that fail to invest in AI risk falling behind in attracting top talent. Conversely, implementing AI prematurely or ineffectively can lead to clinician frustration, increasing burnout and turnover rates. Striking the right balance between innovation and usability is key to maintaining a motivated and engaged workforce.
Finally, health systems must recognize when to abandon AI solutions that fail to deliver meaningful outcomes. Not every AI tool is a good fit for every organization, and some solutions may prove to be more disruptive than beneficial. AI adoption should be driven by its ability to generate tangible improvements in patient care and clinical workflows. If a tool does not demonstrate clear value, health systems must be willing to pivot or discontinue its use rather than force adoption for the sake of staying competitive.
The AI arms race in healthcare is not about simply adopting the most advanced tools—it is about implementing the right tools effectively. Health systems must prioritize seamless integration, usability and real-world outcomes to ensure AI adoption drives meaningful improvements in patient care and operational efficiency. By taking a thoughtful, clinician- and patient-centric approach, healthcare organizations can harness the power of AI while avoiding the pitfalls of premature implementation.
The adoption of AI will be a fundamental part of success in the healthcare industry moving forward. However, success in the AI arms race will not be determined by which organization adopts technology first, but rather by which one implements it in a way that enhances care delivery without compromise. The future of AI in healthcare depends on its support for clinical workflows in ways that enhance and improve patient care while reducing administrative burdens, allowing doctors and nurses to spend more valuable time with patients than ever before.