The story of fragmented care is a common one in healthcare. It’s the story of a patient whose physical recovery from surgery is stalled by undiagnosed anxiety. It’s the story of a family struggling to manage a loved one’s chronic disease, unaware that untreated depression is sabotaging their progress. For decades, the divide between behavioral and physical health has been a silent chasm in our medical system, costing not just billions in duplicative services and avoidable hospitalizations, but also immeasurable human suffering.
For a long time, we acknowledged this problem as an unfortunate reality. Medical records, care teams, and even our payment systems were all designed to keep these two worlds separate. A patient could be receiving world-class care from their endocrinologist and a compassionate, effective therapist, yet the insights from one provider rarely, if ever, made it to the other. The human body and mind, in reality a single interconnected system, were treated as two distinct and unrelated entities.
Today, that paradigm is shifting. The push for whole-person care has moved from a philosophical idea to an operational imperative. This holistic approach, which recognizes that mental health is a fundamental component of physical health, has been shown to improve outcomes for chronic disease management, increase patient engagement, and ultimately, create a more sustainable health system. But bridging this chasm requires more than just a change in mindset; it demands a fundamental change in the technological infrastructure that underpins modern medicine.
The Technology Foundation: More Than Just Connecting Silos
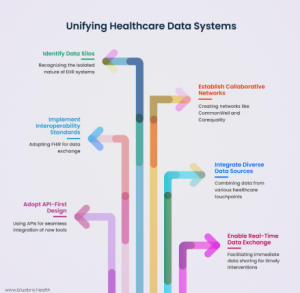
The first, and most critical, step toward unification is breaking down the data silos that have long defined healthcare. Electronic Health Records (EHRs) have been a major leap forward in digitizing patient information, but their design has historically favored isolation over integration. Each system operates like a walled garden, making it difficult for information to flow freely across different clinics, hospitals, and specialties.
Significant progress has been made with the widespread adoption of interoperability standards like FHIR (Fast Healthcare Interoperability Resources), which provides a common language for health data exchange. Collaborative networks like CommonWell Health Alliance and Carequality have also created the on-ramps to a connected healthcare ecosystem. However, true unification requires more than just connecting medical records. It demands that data from every touchpoint—from a therapy session and a primary care visit to social care data and remote monitoring—can be brought together in a purpose-built behavioral health EHR to create a single, comprehensive view of a patient’s health.
The architecture of this integrated system is paramount. The most effective solutions are built on an API-first design, a foundational approach that allows for new tools and technologies to plug seamlessly into existing clinical workflows. This design philosophy is a game-changer because it allows health systems to be flexible and agile. They no longer have to wait for a massive, full-scale EHR upgrade to launch a new program.
Instead, they can layer in new capabilities for behavioral and physical health integration with minimal disruption. Real-time data exchange completes this foundation, shrinking the lag between action and awareness. When a care manager is instantly alerted to a sudden emergency room admission for a patient who was recently diagnosed with a substance use disorder, they can intervene and coordinate care before a crisis escalates.
The AI Catalyst: From Insights to Action
Once this robust data foundation is in place, artificial intelligence becomes the catalyst that transforms raw data into a coordinated, intelligent care delivery system. AI’s true power isn’t just in processing information; it’s in its ability to generate actionable intelligence at the exact moment a care team needs it.
Predictive analytics can separate and stratify patient populations by risk, moving health systems from a reactive to a proactive model. By analyzing a patient’s combined behavioral and physical profiles, AI can highlight those at high risk for future complications. For example, a patient with Type 2 diabetes who also has high scores on a depression screening and a history of missed appointments could be automatically flagged for proactive outreach. This means providers can intervene with a telehealth call or a behavioral health check-in, preventing a potential health crisis from ever occurring.
Beyond prediction, AI can make treatment plans dynamic and adaptive. In a traditional setting, a patient might receive a static, one-size-fits-all recovery plan after surgery. With an AI-powered system, that plan becomes a living document that adapts as new data flows in.
If a patient with a history of PTSD shows an increase in anxiety symptoms during their physical recovery, the system can automatically adjust their care pathway to include a mental health check-in or a referral to a new therapy session. This personalized, responsive approach ensures that care is always aligned with the patient’s evolving needs.
AI also strengthens the capabilities of front-line care providers. Tools integrated into a primary care physician’s workflow can use AI to analyze patient responses and flag subtle signs of depression or anxiety, conditions that are frequently missed in a rushed 15-minute appointment. Furthermore, Natural Language Processing (NLP) can sift through unstructured notes and data across different specialties—like a therapist’s notes and a primary care physician’s narrative—to uncover connections between behavioral symptoms and physical conditions that might otherwise remain invisible.
Designing a Human-Centered Implementation Framework
The most sophisticated technology is useless without a thoughtful implementation strategy. It’s not enough to simply “turn on” an AI system. The process of integration must be human-centered, designed to empower clinicians and improve patient outcomes.
The first phase of implementation should be a deliberate, phased approach focused on integrating data and mapping out workflows. This involves identifying where behavioral and physical health information is siloed and designing the digital pathways to merge them. The second phase involves piloting the AI models with defined patient cohorts. At this stage, it is crucial to focus on bias reduction, ensuring that the models are fair and equitable, and to provide clinicians with the necessary tools and training to use the systems effectively.
Scaling follows once the pilots demonstrate tangible value. As integrated pathways are rolled out to broader populations, the AI models are continuously retrained on new data, becoming smarter and more precise over time. Change management is a continuous effort. Clinicians need reassurance that AI is not a replacement but an assistive technology that will ease their workload by automating redundant tasks and providing them with a more complete view of their patients.
Measuring Success: Beyond the Financials
The success of integrated care and its AI-powered enablers should be measured by a mix of clinical, operational, financial, and experiential metrics.
On the clinical side, clear evidence of success includes improvements in depression screening and follow-up rates, along with better chronic disease management outcomes. From an operational perspective, success is reflected in stronger coordination between care teams, a reduction in redundant tests, and less administrative burden on staff. Financially, health systems with integrated care models often report fewer hospital readmissions and emergency room visits—outcomes that align perfectly with the ideals of value-based care.
But perhaps the most important metric is patient satisfaction. When behavioral health is addressed alongside physical conditions, patients feel seen and heard. They report higher satisfaction and stronger engagement, a reflection of care that treats them as whole individuals, not fragmented cases.
The future of healthcare is a unified ecosystem where technology supports and enhances the human-centered practice of medicine. By strategically leveraging AI to break down silos and provide a single, comprehensive view of the patient, we can move closer to a system that is not only more efficient but also profoundly more humane.