When AI Gets It Wrong in Mental Health Billing
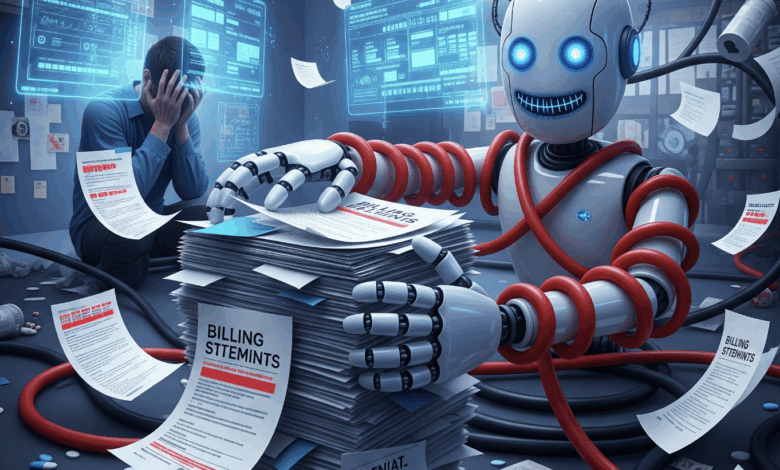
Last Tuesday, a therapist called me in tears. She’d been relying on a popular AI billing assistant and had just lost $3,000 in denied claims. The system had confidently guided her through a submission process for Blue Cross, but failed to account for a crucial Massachusetts specific supervision requirement that any experienced human biller would have caught.
This isn’t a one off mistake. It’s becoming common, and it’s costing mental health providers more than just money.
When a Simple Mistake Costs Everything
In this case, the provider submitted a claim for a 90837 psychotherapy session, a standard 53minute appointment. The expected reimbursement was $150. But the claim was missing a supervision modifier required for her license type in Massachusetts.
That error led to a denial. The appeal took six weeks. She lost not only the reimbursement but also hours of administrative time and the opportunity cost of patient care.
Now multiply that error across dozens of claims per month. Small practices with thin margins can’t afford these kinds of disruptions. And they shouldn’t have to.
The Billing Labyrinth Generic AI Cannot Navigate
Mental health billing isn’t just complex; it’s deliberately difficult. Rules vary by geography, payer type, license, and even time of year. General-purpose AI tools simply aren’t built for that level of chaos.
Take Blue Cross Blue Shield. In Massachusetts, prepayment reviews are often required for certain 90837 codes. But two hours north in New Hampshire, those requirements vanish. Cross into Vermont? You’ll need a new playbook. Same payer. Same CPT code. Entirely different rules.
Now look at Tricare. You’d think a federal program would be consistent. It’s not. TricareEast and Tricare West operate like separate companies, with different provider enrollment rules, prior authorization policies, and billing quirks.
Then there’s the supervision maze. A licensed clinical social worker under supervision must link claims properly to their supervisor. Miss that one step, and you risk invalidating every associated claim. I’ve seen practices lose $15,000 overnight because of a single credentialing mismatch.
And coordination of benefits (COB) issues? They’re silent killers. Payers can claw back payments months after service for COB errors the provider never even saw. Practices already operating paycheck to paycheck simply can’t absorb that kind of financial shock.
Generic AI doesn’t stand a chance in this kind of terrain. It can write emails or summarize data, but healthcare billing requires a level of contextual understanding that these tools just don’t have.
What Specialized AI Actually Accomplishes
When we began developing AI tools inside our company, we didn’t try to mimic ChatGPT or build an all-purpose assistant. We started with our frontline pain points: denial management, SOP access, and hiring.
● Denial Triage Support
Our AI denial assistant distinguishes between CO97 (service bundled with another) and CO16 (missing information). Instead of simply flagging a denial, it proposes appropriate next steps, based on both code definitions and payer-specific behavior.
● SOP and Protocol Memory
Our SOP assistant lives in Slack and can instantly deliver our internal process for verifying benefits for, say, a Texas Medicaid patient, including which portal to use, documentation needed, and common mistakes to avoid.
● Healthcare Specific Hiring AI
We’ve embedded AI into hiring to flag instability (e.g., gaps in employment), software knowledge, and cultural fit for remote work. It doesn’t replace interviews, but it speeds up shortlisting by 80%.
These tools aren’t flashy; they just work. They’re embedded in our workflow, respect compliance boundaries, and improve decision-making without overstepping.
The Hidden Cost of Misapplied AI
The damage from general AI in healthcare isn’t theoretical; it’s measurable.
Many tools don’t understand Electronic Remittance Advice (ERAs). They can’t navigate payer portals. They don’t differentiate between denials that can be appealed and those that reflect credentialing issues that cannot. And they definitely don’t know which modifiers are required for a Licensed Professional Counselor in Pennsylvania or which codes are rejected by Optum in Arizona.
Worst of all, these tools often sound confident when they’re dead wrong. They offer inaccurate guidance with authority, leaving staff confused and billing departments picking up the pieces.
This erodes trust and costs time. For mental health practices already stretched thin, that inefficiency is unsustainable.
The Right Way to Build Healthcare AI
Here’s how we approached building internal tools that actually work in healthcare billing:
● Document Real SOPs
We started with our existing protocols, not hypothetical workflows. That meant capturing exactly how we verify benefits, respond to denials, or prepare for audits.
● Train AI on Real Claims Data
We used anonymized, HIPAA-compliant historical data—including payer responses, denials, and appeals to build relevant training models.
● Integrate with Systems We Already Use
Our tools connect with Google Sheets, EHR platforms, and email. No duplicate entry. No friction.
● Maintain Human Oversight
AI doesn’t replace our team, it supports them. Humans make the final call. AI reduces mental load.
Principles That Actually Work
From what we’ve learned, effective healthcare AI must follow these rules:
● Specificity drives accuracy: General AI trained on Reddit threads or Wikipedia won’t outperform models trained on claims, SOPs, and payer data.
● Workflow integration is mandatory: Tools must align with how billing teams actually work.
● Compliance comes first: HIPAA isn’t optional. Tools must be privacy-conscious from the start.
● Humans still matter: AI’s role is to simplify, not substitute. Judgment, empathy, and strategy still require a human mind.
What Practice Owners Should Ask Before Using AI
Ask yourself:
● Does this AI understand my payer mix and credentialing requirements?
● Has it been trained on real claims, not just general healthcare info?
● Does it reduce workload, or shift the burden elsewhere?
● Does it integrate with the platforms my team already uses?
If the answer to any of those is “no,” the tool may not be ready for your practice, and it could do more harm than good.
The Bottom Line
The mental health billing landscape is more complicated than ever. Practices need tools that alleviate, not add to, the burden. Specialized AI tools, built for the actual chaos of healthcare reimbursement, are no longer a luxury. They’re a necessity.
Generic AI can impress in a demo. But specialized AI keeps the lights on, the staff paid, and the providers focused on what matters, patient care.