The clinical trial model is showing its age. Drug development costs have ballooned. Timelines regularly stretch beyond what sponsors or patients can sustain. And despite scientific advances, the majority of drug candidates still fail in trials.
During trial conduct, sources of challenges are numerous, from patient response heterogeneity, unexpected dropouts, and the placebo effect routinely derail even the most well-designed studies. Now, researchers and trial sponsors are asking: how can we better anticipate and manage these human variables that derail clinical progress?
Artificial intelligence (AI) holds promise, but it must evolve beyond operational automation. To meaningfully improve success rates, AI must help us better understand the people behind the data.
The rise of predictive behavioral modeling in clinical trials
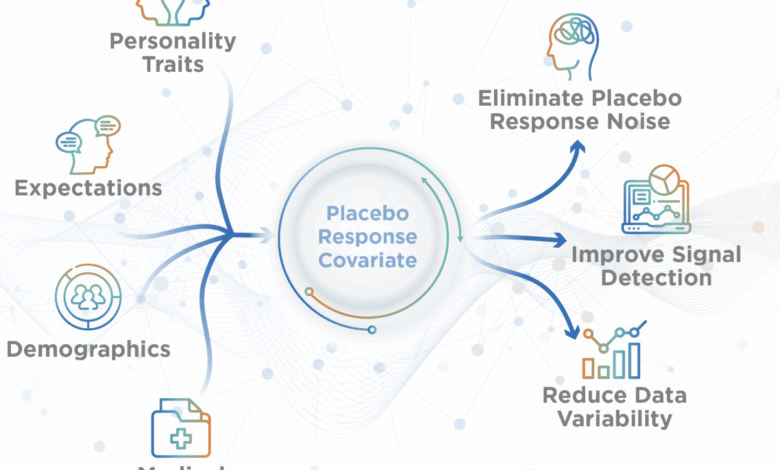
Predictive behavioral modeling is a rapidly growing area of AI focused on using psychological and contextual data to forecast how patients are likely to behave within a clinical trial. Rather than relying solely on biomarkers or medical histories, predictive behavioral modeling considers mindset, emotional status, social factors, and personality traits.
This means being able to anticipate, and act on, issues like nonadherence or poor adherence, early dropout, or heightened placebo responsiveness. These models are not general AI tools operating on massive datasets of secondary information. They rely on high-quality, patient-specific data gathered through validated assessments and psychometric tools.
This shift from purely biological to behavioral data reflects a broader evolution in research. It aligns with growing interest from regulators in patient-reported outcomes and lived experience as critical dimensions of therapeutic effectiveness.
Why behavioral modeling is a game changer
What makes behavioral modeling so powerful is its ability to predict, and in some cases prevent trial failure, by identifying risks early and tailoring interventions accordingly. By flagging patterns linked to dropout or inconsistent reporting, it allows researchers to adapt earlier and with more precision.
Psychological traits can signal how likely a patient is to stay engaged in a study, how they might respond to a placebo, or how they’ll report side effects. These human factors have long been treated as unpredictable noise in clinical research. Now, they’re becoming central to how trials are designed, conducted, and analyzed.
Importantly, behavioral data does not replace biological data. It complements and enhances it. Behavioral modeling allows researchers to assess the “why” behind the “what”. This creates a more complete and patient-centered view of efficacy and safety.
Studies have shown that incorporating behavioral data can enhance assay sensitivity in clinical trials, potentially improving statistical significance by accounting for patient variability. This approach may help in selecting the right compound or disregarding an ineffective one. Incorporating analysis adjustments with more patient characteristics is more informative and will increase the study’s power. This may transform previously non-significant findings into statistically significant ones, or help a sponsor confidently terminate a development program based on clear behavioral insights, thereby saving valuable time and resources
Using behavioral AI in trial design and execution
Behavioral models are more than analytic tools. They enable real-time adaptability. By forecasting challenges such as poor adherence, difficulty following study procedures, early dropout risk, or likelihood of placebo response, predictive behavioral modeling allows teams to proactively support at-risk patients and adjust site strategies or trial protocols accordingly.
Behavioral AI can help identify patients who are more likely to meet protocol demands, reducing attrition. In execution, it can spot early warnings signs of disengagement, allowing the research teams to step in with support. And in efficacy analysis, it can help ensure that statistically significant outcomes also reflect meaningful patient benefit.
This ability to model, monitor, and adapt based on behavior gives sponsors a competitive advantage: improved operational efficiency, proactive rather than retrospective trial management, stronger data integrity, and faster, more informed decisions about whether to advance, pause, or terminate a program.
Regulatory considerations
As predictive behavioral modeling becomes more widely used, so does the need for strong scientific and ethical guardrails. Transparency is key. Building the model is not the hardest part. Thorough and unbiased evaluation is key to ensuring consistent performance, especially in real-world populations. The validation process is what can make or break a model.
Regulatory agencies like the FDA and EMA echo this view, emphasizing that transparency, interpretability, and validation should be proportional to the level of risk associated with an AI model and its intended use. The FDA issued a Risk-Based Credibility Assessment Framework for any AI used to support regulatory decisions making.
The specific data requirement prevents behavioral models from relying on historical records or publicly available data sources. Thus, data collection plays a critical role in the success of a behavioral model: collecting the correct data from a representative population. This data collection process is an integral part of the Risk-Based Framework proposed by the FDA.
Above all, the best use for these models might not be autonomous decision-making, but supporting, not replacing, human judgment. Their value lies in patterns, clarifying complex dynamics and enabling more informed, patient-centric decision making.
The future of AI in clinical trials
The use of AI is becoming a critical element of clinical research from protocol development to finding the right patients for the right protocol, data management, and more. In the years to come, AI will continue moving deeper into the heart of clinical trials and will play a more active role in trial conduct, efficacy evaluation, and participant engagement.
We anticipate a shift toward more representative AI models, those that reflect the true diversity of the patient population, including behavioral heterogeneity. Behavioral AI offers a way to incorporate real-life factors that influence how patients engage in clinical trials, such as stress, motivation, life context, and social determinants of health, helping to design more inclusive studies with broader relevance and stronger generalizability.
We also expect a broader cultural shift across the clinical research industry. Success will no longer be defined solely by biological markers. It will depend on understanding the human experience of treatment, how patients feel, whether they function better, and if they remain engaged across the trial. Understanding the lived experience of treatment will become essential.
Re-centering the human in clinical research and beyond
The future of clinical trials demands more than faster recruitment or more data points. It requires re-centering the human being in clinical trials. Predictive behavioral modeling offers a path to do just that by quantifying the influence of emotion, personality, and context into the research process. Predictive behavioral modeling helps ensure that the impact of various factors on trial measures and execution supports the timely and efficient delivery of innovative treatments to the patients who need them most.
We are all human. We don’t respond to stress or treatment in identical ways. If we truly want to be patient centric, we must understand the human part of the patient.
It is equally important in real life to support patients by providing tailored patient engagement strategies. Improving adherence to treatment and medical procedures can only be beneficial, primarily for the patient and for the health economic system.
Adopting predictive behavioral modeling is not just a technological upgrade. It’s a mindset shift, a call to see patients as full participants in clinical research, not just data sources. And in doing so, it may be the key to unlocking safer, smarter, and more successful trials.





