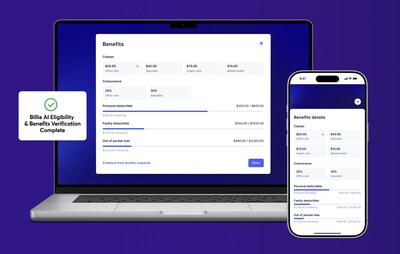
SAN FRANCISCO, Oct. 30, 2025 /PRNewswire/ — Collectly, the AI-powered technology company specializing in patient billing, revenue cycle management (RCM), and engagement solutions, today announced the launch of Billie AI Eligibility & Benefits, a new suite of AI-driven products designed to automate eligibility verification and deliver real-time copay calculation and collection.
With this launch, Collectly continues to expand its mission of building a modern, AI-powered end-to-end patient financial experience — part of its broader vision to redefine patient RCM & engagement, empowering providers to deliver transparency and efficiency from intake to payment while creating a simpler, more connected patient financial experience at every step of care.
Early adopters like Medical Associates of Northwest Arkansas (MANA) — one of the region’s largest physician-owned, multi-specialty medical groups — are already seeing measurable improvements in automation and efficiency:
“We transitioned to Collectly’s AI eligibility and benefits verification after using another solution that just wasn’t keeping up. With Collectly, the resolution rate started higher and continues to improve. This means our team is seeing fewer and fewer manual interventions week over week.”
— Darron Mitchell, Administrator of Business Operations, Medical Associates of Northwest Arkansas (MANA) (https://mana.md/)
A Persistent Challenge in Healthcare Finance
Determining eligibility and benefits remains one of the most time-consuming, error-prone steps in the revenue cycle. For each patient visit, staff must still verify coverage details, determine whether insurance will cover part or all of the visit, confirm deductible or out-of-pocket maximum status, and identify any prior authorization needs.
This process — often handled through manual review of cumbersome 271 EDI files, payer portals, or time-consuming phone calls — slows down front-office operations and leaves room for costly human error. Many RCM leaders describe it as a “15-minute-per-patient” bottleneck that directly impacts cash flow and patient satisfaction.
Automation That Eliminates Manual Work
Collectly solves that problem with automation designed to eliminate manual effort altogether — transforming what used to be an administrative burden into a fully hands-free process.
The platform automates the entire eligibility and benefits verification loop — from verification and copay calculation to refunds and follow-ups — removing the repetitive, manual steps that have traditionally slowed down front-office teams. In real-world deployments, teams see the workflow drop from roughly 12 minutes to near-zero staff time per patient, with significantly fewer portals, calls, and errors.
“Each health benefit check can cost providers $3–$10 in staff time alone,” said Max Mizotin, CTO of Collectly. “This is the time it takes staff to interpret a patient’s benefit check details, compare it to their appointment information, and pull out critical details such as their coverage status, expected copay, deductible, coinsurance, prior authorization requirements, network restrictions, and more.”
“Collectly drives that time toward near-zero by fully automating this work with a new AI agent trained to gather data from provider and payer systems, interpret this data in the context of the patient’s upcoming appointment, and surface the most important and relevant information directly for patients and staff.”
“The automation doesn’t end there, Collectly also handles allocations, credits and refunds automatically following the organization’s policy. What once required multiple manual touches now happens in seconds, with human review only when absolutely necessary. On top of that, we’ve seen class-leading first-pass accuracy — up to 80% — even in complex specialties like mental health, where inconsistent payer responses and nuanced coverage logic demand advanced AI interpretation.”
“Eligibility and benefits have historically been bottlenecks that slow down cash flow and frustrate both patients and staff,” said Levon Brutyan, CEO of Collectly. “By adding AI-powered Eligibility and Benefits to our platform, we’re removing guesswork, reducing administrative burden, and giving providers and patients clarity from the very start of the care journey.“
A Smarter, AI-Driven Solution
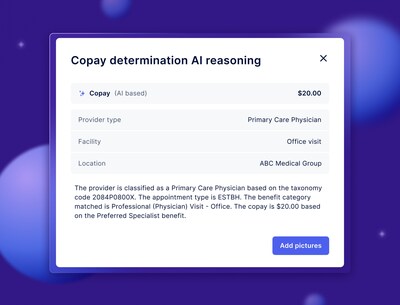
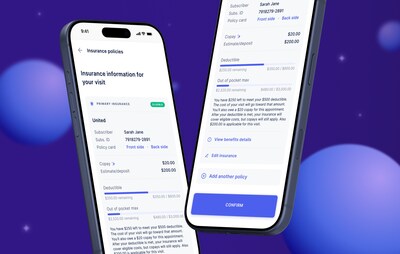
Collectly’s AI Eligibility & Benefits solution reimagines this process by automating verification of insurance coverage and instantly surfacing patient-specific financial information in a usable, easy-to-understand format for both staff and patients.
“For years, the way payers structured EDI data has created unnecessary complexity for providers — those files were never designed with provider usability in mind,” said Kevin Lunn, VP of Product at Collectly. “With Billie AI Eligibility & Benefits, we’ve built a system that bridges that gap — transforming fragmented data into a connected, automated process that just works, requiring far less training, far less manual rework, and minimal human intervention.”
Leveraging advanced AI models, the solution often delivers up to a 30% improvement in accuracy compared to traditional systems, allowing providers to identify coverage details, copay and deductible amounts in real time — before care is delivered.
Unlike traditional systems that simply return raw 271 data, Collectly’s AI leverages a large language model (LLM). The model analyzes the 271 response alongside taxonomy codes, CPT and ICD codes, and historical claim trends to identify gaps, predict likely coverage, and flag edge cases such as specialty carve-outs. When a payer’s response is incomplete or ambiguous, the LLM applies learned reasoning patterns from similar claims and payer behaviors to infer missing details and provide high-confidence results.
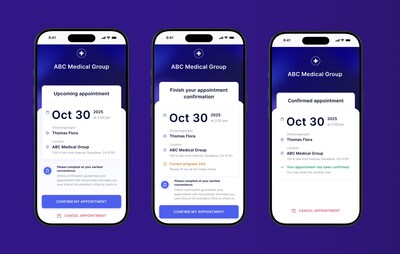
A More Automated, AI-Powered Patient Financial Journey
With this release, Collectly further strengthens its end-to-end, AI-powered financial experience — adding deeper automation, intelligence, and interoperability to every step of the patient journey.
- Pre-Service: AI Eligibility & Benefits with real-time copay calculation and collection
- Point of Service: Integrated digital and in-person payment options, plus terminal-based data capture to automatically update patient contact details like mobile phone and email in the EHR
- Post-Service: AI-driven billing automation, omnichannel communication, self-serve payment plans, and Billie — Collectly’s 24/7 AI RCM agent that resolves ~85% of patient billing inquiries
Behind the scenes, Collectly’s deep EHR interoperability and smart read/write capabilities ensure data flows seamlessly across systems — syncing eligibility, benefits, payments, and patient information in real time for a unified financial record.
This unified workflow gives providers a connected, intelligent ecosystem for financial engagement — one that enhances operational efficiency, accelerates payments, and delivers a patient-friendly experience that matches the quality of clinical care.
Proven Results and Early Adoption
Early adopters of Collectly’s Billie AI Eligibility & Benefits report tangible improvements in both financial performance and patient satisfaction, including:
- Dramatically reduced staff workload through automation that eliminates manual eligibility checks and follow-up work
- Fewer claim denials through accurate, real-time eligibility and benefits verification
- Faster collections as patients pay known copays at or before their visit
- Higher patient satisfaction driven by transparent, upfront financial communication
“Providers tell us all the time: patients love their clinical care but get frustrated when billing surprises appear,” said Bartek Woroniecki, VP of Growth at Collectly. “With Billie AI Eligibility and Benefits, we’re addressing that frustration at the source — bringing clarity and automation to the first step of the financial journey so providers can focus on care, not collections.”
For a deeper look at how the AI Agent for Eligibility & Benefits transforms this workflow, learn more and request info here: www.collectly.co/billie-ai-eligibility-and-benefits
Enterprise-Grade Security and Compliance
Collectly’s platform is SOC 2 compliant, HITRUST certified, HIPAA compliant, and PCI DSS compliant, ensuring that all healthcare, eligibility, benefits, and payment data are handled with the highest levels of security and privacy.
About Collectly
Collectly is an AI-powered technology company specializing in patient billing, revenue cycle management, and engagement solutions. Integrated with 20+ leading EHRs, Collectly helps healthcare organizations streamline financial workflows, accelerate cash flow, lower cost to collect, and deliver a modern, patient-friendly billing experience.
Trusted by over 3,000 healthcare organizations across the U.S., Collectly has processed more than $1 billion in patient payments.
To Learn More
To learn more about Collectly’s AI-powered RCM and engagement platform — and how it helps healthcare organizations modernize financial workflows, accelerate cash flow, and elevate the patient experience — visit or contact Collectly at www.collectly.co.
Media Contact
Bartek Woroniecki
Vice President, Growth
Collectly
[email protected]
408.466.5417
www.collectly.co
View original content to download multimedia:https://www.prnewswire.com/news-releases/collectly-expands-end-to-end-ai-powered-patient-financial-experience-with-launch-of-billie-ai-agent-for-eligibility–benefits-302599170.html
SOURCE Collectly