Healthcare credentialing in the U.S. is on the verge of a much-needed upgrade. A patent-pending innovation currently under research explores how AI and blockchain technology can modernize verification processes, reduce onboarding delays, and strengthen trust across the U.S. healthcare ecosystem.
Srinivas Baipalli, a lead software engineer, is actively working on research and developing a next-generation platform that addresses a long-standing issue in the U.S. healthcare system: the slow and error-prone process of verifying and credentialing healthcare providers.
This innovation leverages artificial intelligence and blockchain technology to enable real-time provider verification. The goal is to eliminate inefficiencies that delay care, increase administrative burden, and create compliance risks.
THE CHALLENGE
Credentialing healthcare providers, which involves confirming their qualifications, licenses, work history, and any disciplinary actions, remains a slow, manual, and error-prone process. Many healthcare organizations still depend on outdated methods such as paper forms, spreadsheets, and siloed systems that do not communicate with each other. These legacy systems require administrators to collect and verify information from multiple sources, often by phone, fax, or email. Because the data is scattered and disconnected, even a small error or missing document can cause significant delays. This not only postpones when a provider can begin seeing patients but also increases the risk of inaccurate or outdated information making its way into patient-facing systems. The result is a system that is burdensome for administrators, frustrating for providers, and potentially unsafe for patients.
“I started working on this after witnessing firsthand how outdated systems affect everything from patient access to reimbursement,” said Srinivas Baipalli, the system’s inventor. “We need to shift from periodic checks to continuous AI-driven trust.”
Baipalli, a Lead Software Engineer, began his research after reviewing recent federal and private audits from agencies such as the Office of Inspector General and the Government Accountability Office, which identified systemic issues in provider data management.
THE PROPOSAL
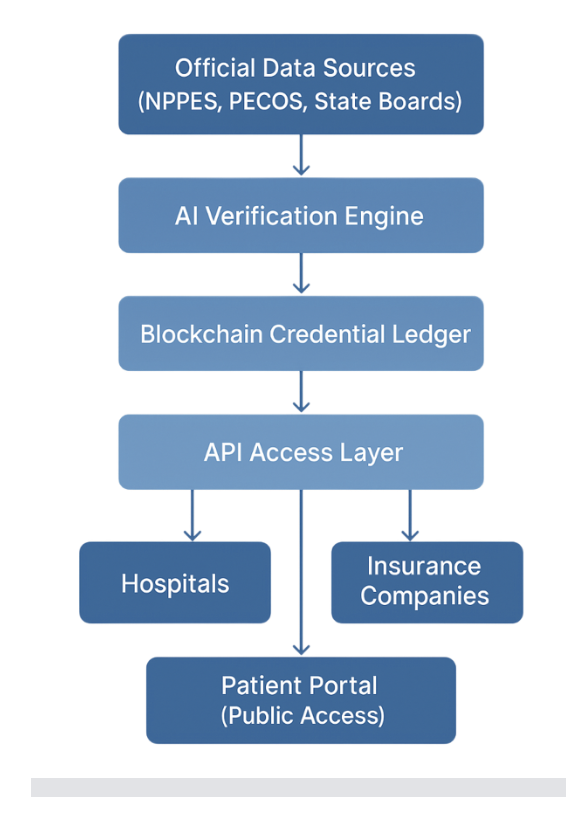
The platform Baipalli is researching and developing uses artificial intelligence to continuously verify provider credentials from authoritative data sources such as NPPES, PECOS, and state licensing boards. Verified records are securely stored using blockchain, providing transparency and ensuring data integrity.
Key features include:
- Real-time credential verification and automated onboarding
- Blockchain-based audit logs for accountability and compliance
- API integrations that allow hospitals, insurers, and public directories to access verified data
This approach gives healthcare stakeholders immediate access to accurate provider information without relying on manual processes or delayed third-party verifications.
MEETING THE CHALLENGE
The research-driven system is designed to meet the needs of multiple user groups:
- Government programs such as Medicare and Medicaid can use it to prevent fraud and streamline compliance workflows.
- Private health systems and insurers can reduce time to onboard providers and improve data accuracy.
- Patients and public directories can access up-to-date provider information that improves trust and transparency.
“Credentialing today is filled with inefficiencies,” Baipalli said. “This platform creates a foundation of trust by making verification secure, scalable, and instantaneous.”
RESULTS AND NEXT STEPS
Based on workflow analysis and system design research, the platform has the potential to reduce provider onboarding time by more than 60 percent. Simulations also point to fewer credentialing errors, improved data consistency, and reduced administrative overhead. These findings are grounded in comparisons between current manual processes and the efficiencies enabled by automated verification and blockchain-based logging.
Baipalli is continuing to develop the platform and collaborate with stakeholders to refine its integration, expand AI validation capabilities, and align it with federal and industry compliance requirements.
“This work is not just about technology,” he said. “It is about building a smarter and more reliable healthcare infrastructure that benefits everyone; patients, providers, and payers alike.”