The shift from smart widgets to agentic workflows
Most organizations meet AI through a feature: a transcript button here, a summarizer there. Useful? Sure. Transformational? Not really. The bigger unlock is agentic AI—systems that don’t just predict or label, but that capture signals, decide with context, and then act inside your operations with auditable guardrails.
Healthcare admin is a perfect stress test: complex rules, brittle integrations, and human time spent on preventable work. If agentic AI can make a dent here, it can make a dent almost anywhere. The playbook below is sector-agnostic, but I’ll ground it in clinical operations because the stakes (and the waste) are apparent.
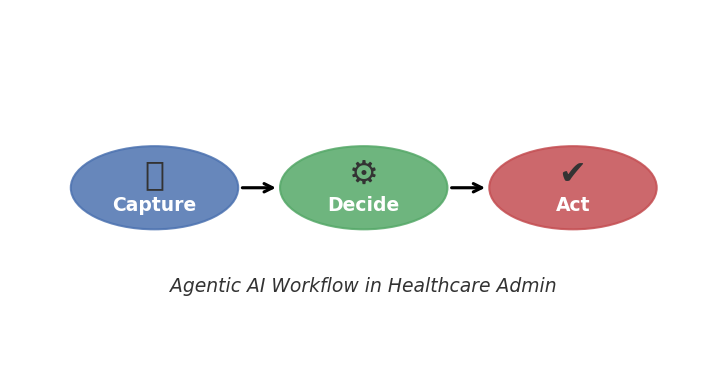
A simple framework: Capture → Decide → Act
Agentic AI works best when you design from flow, not features. Map the exact path a task takes today, then place AI where it turns friction into momentum.
1) Capture (Signals): Turn messy inputs into structured signals that the rest of the system can use.
2) Decide (Policy + Context): Apply business rules and model inferences to pick the following best action.
3) Act (Do the Work): Execute the action in your systems—create/update records, send a message, file a claim—with logs and human-in-the-loop on risky steps.
Do this well, and you replace swiveling between screens and ‘just checking on this’ emails with closed-loop execution.
Five high-impact healthcare admin use cases
1) Ambient scribing → structured notes
Capture: Audio from the clinical encounter is transcribed, medical entities are recognized, and draft SOAP notes are composed.
Decide: Apply specialty-specific templates, insurance documentation rules, and clinician preferences. Flag missing elements.
Act: Generate a draft note in the EHR; the clinician approves/edits in seconds instead of writing from scratch.
Why it matters: The number of minutes per visit drops, and charting after hours shrinks. The win isn’t ‘AI wrote something,’ it’s consistently structured notes.
2) Eligibility and pre-auth as a background process
Capture: Appointment creation triggers insurance eligibility checks and pulls plan details.
Decide: Policy rules determine whether pre-auth is required based on CPT/diagnosis and payer quirks.
Act: If needed, assemble a pre-auth packet from the chart and submit; set a timer to check status; notify the front desk only for exceptions.
Why it matters: By avoiding last-minute surprises at check-in, you’ll experience fewer reschedules, fewer write-offs, and a calmer front desk. The goal is to generate more revenue consistently. This is a professional organization that relies on billable hours, so let’s make sure that capacity is at its highest levels at all times.
3) Claim pre-scrubbing and denial prevention
Capture: After each visit, the system assembles claim lines, NPI/taxonomy, modifiers, and documentation links.
Decide: Run rules for common edit sets (payer-specific modifiers, frequency limits, LCDs), and score denial risk.
Act: Auto-correct safe items and route high-risk claims to an exception queue.
Why it matters: You improve first-pass acceptance and cut the rework loop that drags A/R days up.
4) Exceptions routing that respects human attention
Capture: Tickets, denials, patient messages, and portal payments stream into one queue with metadata.
Decide: Classify by effort/impact; apply policies.
Act: Auto-resolve low-risk cases; route the rest to the smallest qualified group with a recommended action and deadline.
Why it matters: Staff focus on the next best thing, not the one that demands immediate attention.
5) Patient pay follow-up that’s helpful, not harassing
Capture: Balances, comms preferences, and recent interactions.
Decide: Personalize cadence, suggest a payment plan, pause if there’s an active dispute.
Act: Send clear statements with plain-English descriptions; provide a one-tap way to ask questions or fix coding issues.
Why it matters: Collections improve without torpedoing patient satisfaction.
Metrics that actually move
If AI is working, the operating metrics will tell you before the anecdotes do. A practical scorecard:
– Minutes saved per visit
– First-pass acceptance rate and denial trends
– Days in A/R and % claims > 60 days
– Exceptions backlog age
– Front desk load leveling
– Patient comms satisfaction
Guardrails: trust is a feature
Agentic AI without governance is just fast chaos. Three non-negotiables:
– PHI & privacy
– Human-in-the-loop (HITL)
– Explainability & audit
The 30/60/90 rollout plan
Days 0–30: Map & pilot
Days 31–60: HITL → partial autonomy
Days 61–90: Scale the pattern
Seven pitfalls to avoid
1) Feature-first thinking
2) No owner
3) Model worship
4) Over-automation
5) Unclear policies
6) Ignoring edge cases
7) Silent failures
Beyond healthcare: a template you can reuse
The same pattern shows up in finance ops, customer support, and supply chain. In every case, the breakthrough is the closed loop.
What the C-suite should ask
– Where does work stall today?
– What decisions are we standardizing?
– How will we prove it works?
– What’s our HITL plan?
– How fast can we iterate?
The bottom line
Agentic AI isn’t about replacing people; it’s about giving teams their time back and making the remaining work count.


